Often, weighing yourself is a big part of having an eating disorder. Sometimes many, many times a day. That number on the scale, and the one inside your pants, comes to drive how you feel, what you do, how you eat, and how you view yourself. Suddenly, that number on the scale seems to be driving everything.
But, it feels reassuring. It feels comforting to know what is happening with that number (though, let's be honest, only as long as it is not going up!). Your eating disorder is reassured by that illusion of control. So, it is hard to let go of the behavior. I have had numerous new patients argue with me that seeing their weight helps, not hurts--mostly because the client is too scared to not know the number. Being weighed by us is often a significant area of stress, and sometimes conflict.
And, of course, this is another area of great debate in the field. Should we show weights or hide weights. Do they hurt, or do they help? And how do you know from patient to patient?
At UCED, we do blind weights, for those with whom we need to do weights. Why? Because we also teach intuitive eating. And, weighing yourself and becoming an intuitive eater are pretty much diametrically opposed (which is why we do not weigh people who are practicing intuitive eating). But why is it so unlikely to work if you both weigh yourself and try to become an intuitive eater? Intuitive eating is based on trusting your body and learning to follow your body's cues. The goal is to eat when you are hungry, stop when you are full, and eat a variety of foods.
Enter, the scale. You jump on that "wonderful" little thing and it gives you a number. What if that number is higher than you want it to be? Chances are you will automatically change your eating behavior to compensate. You will restrict the amount you are eating, or the range of foods you allow yourself. And, as we have covered before, that restricting has a very high chance of then leading you to overeat. And the cycle of disordered eating continues. You are quickly taken right away from from following your body's cues, and intuitive eating has gone out the window.
So, what do we recommend? I highly recommend getting rid of your scale in the most glorious fashion possible. I have had patients confirm that scales don't bounce when dropped from significant heights and they do shatter when hit with another solid object! Send your scale out with a bang! Or, give it to a loved one so they can make it disappear. Take it to your therapist/dietitian/doctor. Or, put it in the garbage yourself, and wave good-bye.
Think of the freedom that can come when your mood and behavior is not dictated by a number on a scale. We are all much more than a number, and the number says absolutely nothing about us as people.
Thursday, December 5, 2013
Monday, December 2, 2013
UCED's Treatment Approach for Adolescents with Eating Disorders
For the past couple years, there has been a lot of research going into, and professional debate regarding, the appropriate treatment of adolescents with eating disorders. Eating disorder treatment, and the mental health field in general, is a hard field when it comes to finding concrete answers as to what is the best approach for treatment. In general, the focus is on identifying empirically/research supported treatments, and then using clinical judgement and skill to identify what will work best for a particular individual.
Recently, most of the focus in treatment of adolescents has been on Family Based Treatment (FBT), which is also known as Maudsley Method. Lock and LeGrange are the main forces behind FBT here in the US, and there are ongoing trials continuing to assess this treatment approach. The mindset behind the approach is keeping adolescents at home, rather than sending them to inpatient/residential treatment centers. Treatment centers certainly have their benefits and are needed in some cases, but our stance here at UCED is that every adolescent (and adult) should first be able to try outpatient treatment at home, prior to being sent to an inpatient/residential program.
One of the major tenets of FBT is the idea that parents know how to feed their children. If you go back in the history of the understanding of EDs, unfortunately, you will find a lot of blame on parents and families. The field as a whole no longer has this attitude towards families, but some long-held beliefs are hard to get past. Fortunately, FBT has shown that many adolescents can get better at home, with their families. However, as with any therapeutic approach, one size does not fit all.
Our approach with adolescents is to first give the teenager a chance to show they have the motivation to get better on their own. So, first we give them the opportunity to make healthy choices regarding food, with the support of their parents. A surprising number of teenagers actually will choose to get better without invasive intervention--a testament to the maturity of these young men and women, and their awareness that the ED is not serving them well. Because adolescents live at home and are supported primarily by their parents, in addition to friends, we involve parents in therapy frequently; typically every other session, although some teenagers choose to have their parents involved in every session. This approach, which teenagers typically are not thrilled to hear about initially, allows us to avoid the risk of the ED "splitting" the treatment team and the parents. Fortunately, most teenagers quickly realize family therapy isn't THAT BAD and come to accept it pretty quickly. (Sometimes parents end up disliking it more than the teenagers!)
If, with this structure, the teen remains unable to do what he/she needs to do in terms of food and activity, we transition to more of an FBT approach, which provides the parents with much more say in what the child is eating and doing. This is a tough transition for some teenagers, as the last thing they want is for parents to tell them what to do! However, on the flip side, this can provide motivation to do what they need to with food, so they can regain some control. This approach is often difficult for parents because they find themselves feeling pulled to "go easy" on their teen, which unintentionally ends up as negotiating with the eating disorder and allowing it to get away with ED behaviors. Therefore, parents need a lot of support in supporting their teens during this phase of treatment. Fortunately, there are a number of resources for parents in this situation; some include:
Recently, most of the focus in treatment of adolescents has been on Family Based Treatment (FBT), which is also known as Maudsley Method. Lock and LeGrange are the main forces behind FBT here in the US, and there are ongoing trials continuing to assess this treatment approach. The mindset behind the approach is keeping adolescents at home, rather than sending them to inpatient/residential treatment centers. Treatment centers certainly have their benefits and are needed in some cases, but our stance here at UCED is that every adolescent (and adult) should first be able to try outpatient treatment at home, prior to being sent to an inpatient/residential program.
One of the major tenets of FBT is the idea that parents know how to feed their children. If you go back in the history of the understanding of EDs, unfortunately, you will find a lot of blame on parents and families. The field as a whole no longer has this attitude towards families, but some long-held beliefs are hard to get past. Fortunately, FBT has shown that many adolescents can get better at home, with their families. However, as with any therapeutic approach, one size does not fit all.
Our approach with adolescents is to first give the teenager a chance to show they have the motivation to get better on their own. So, first we give them the opportunity to make healthy choices regarding food, with the support of their parents. A surprising number of teenagers actually will choose to get better without invasive intervention--a testament to the maturity of these young men and women, and their awareness that the ED is not serving them well. Because adolescents live at home and are supported primarily by their parents, in addition to friends, we involve parents in therapy frequently; typically every other session, although some teenagers choose to have their parents involved in every session. This approach, which teenagers typically are not thrilled to hear about initially, allows us to avoid the risk of the ED "splitting" the treatment team and the parents. Fortunately, most teenagers quickly realize family therapy isn't THAT BAD and come to accept it pretty quickly. (Sometimes parents end up disliking it more than the teenagers!)
If, with this structure, the teen remains unable to do what he/she needs to do in terms of food and activity, we transition to more of an FBT approach, which provides the parents with much more say in what the child is eating and doing. This is a tough transition for some teenagers, as the last thing they want is for parents to tell them what to do! However, on the flip side, this can provide motivation to do what they need to with food, so they can regain some control. This approach is often difficult for parents because they find themselves feeling pulled to "go easy" on their teen, which unintentionally ends up as negotiating with the eating disorder and allowing it to get away with ED behaviors. Therefore, parents need a lot of support in supporting their teens during this phase of treatment. Fortunately, there are a number of resources for parents in this situation; some include:
- aroundthedinnertable.org
- maudsleyparents.org
- feast-ed.org
Finally, there are some teenagers whose ED is so deeply entrenched that inpatient/residential treatment is what is needed. Fortunately, there are very solid adolescent treatment programs in the US, many of which use the FBT approach. At that point, we will help facilitate the teen's admission to a treatment program, and provide ongoing support for the family, as there is still work to be done to make for a successful transition back home.
It is terrifying to have a teenager with an eating disorder. Parents spend a lot of time blaming themselves and trying to figure out what they did wrong. Eating disorders are not so simple as to be caused by one thing, including parents and families. But, by working together, the teen and parents can rid the family of the eating disorder, and strengthen their bonds.
Tuesday, November 26, 2013
Using Intuitive Eating During the Holidays
--by Nicole Holt, RD
The holiday season can be a difficult
time of the year for those who struggle with an eating disorder. It is a time
of the year where family gatherings, work parties, and holiday activities are
often centered on food and impressing others. On the other hand, the holidays can
be an opportunity to stand up to your eating disorder and practice intuitive
eating skills. Let’s go over some intuitive eating concepts to help you feel
confident as we enter the holiday season.
As an Intuitive Eater, you know:
- · If you restrict your intake throughout the day to compensate for a dinner party, you are most likely going to be overly hungry at the party and eat until uncomfortably full.
- · If you eat past fullness, do not panic. The feeling of fullness will likely pass in less than a half hour. In the meantime, you can distract yourself with a conversation about gratitude, or a holiday song!
- · It is your right to honor your fullness and say "no thank you" to seconds or dessert.
- · If you want seconds, you are free to eat them without feeling guilt, judgment or the need to exercise, or purge, to compensate.
- · All foods fit in a healthy diet, including stuffing, pie, and whatever else our society labels as unhealthy!
- · You are the expert on your body. Nobody can feel your hunger and fullness but you.
Being an intuitive eater doesn’t mean
you are perfect. Sometimes it means that you eat more because it tastes good.
It can also mean creating an escape from an eating situation because you are
overwhelmed and need a minute to yourself. Whatever it may be, have faith in
your intuitive eating skills this holiday season.
Thursday, November 21, 2013
Equine Therapy in Eating Disorder Treatment
My interest in animal-assisted therapy began with the puppy-love-of-my-life, Shadow. I became the very honored owner of Shadow, a rescued shiba inu, in May 1999. Although we did not know her history, it quickly became evident she was likely neglected, and potentially abused. I was in graduate school at the time, and Shadow was my first dog. She quickly became the (puppy) love of my life and our bond grew to be very strong. During graduate school, once a semester, she was seen in class, helping me to teach learning theory principles to my Intro to Psych students.
 1. In my opinion, "the best" equine assisted therapy is about the relationship with the horse. It is not using the horse as a "tool," but instead as a co-therapist. Eating disorders have the impact of disconnection, from oneself and from others. For various reasons, human relationships can become threatening, yet that with an animal can be safe. The horse as co-therapist can help facilitate reconnection: with one's emotions, with one's physical body, with relationships in general, and with others in the client's life. When one has an eating disorder, they often cut themselves off from the head down. The body is often ignored at best, and rejected at worst. Well, imagine trying to engage on the ground with a very large animal, without being present in one's body. To take it one step further, imagine trying to sit upon a horse, or ride a horse, without being connected. As you can imagine, these things would be very difficult, so interaction with a horse can challenge that disconnection in very real, and powerful, ways.
1. In my opinion, "the best" equine assisted therapy is about the relationship with the horse. It is not using the horse as a "tool," but instead as a co-therapist. Eating disorders have the impact of disconnection, from oneself and from others. For various reasons, human relationships can become threatening, yet that with an animal can be safe. The horse as co-therapist can help facilitate reconnection: with one's emotions, with one's physical body, with relationships in general, and with others in the client's life. When one has an eating disorder, they often cut themselves off from the head down. The body is often ignored at best, and rejected at worst. Well, imagine trying to engage on the ground with a very large animal, without being present in one's body. To take it one step further, imagine trying to sit upon a horse, or ride a horse, without being connected. As you can imagine, these things would be very difficult, so interaction with a horse can challenge that disconnection in very real, and powerful, ways.
2. Trust: Let's face it; horses are at least 900 pounds, and taller than us. They physically present a challenge to trust. But they will quickly illustrate the desire and motivation to trust us as humans. And that can be so powerful to those who have learned to distrust others.

3. Mirroring: One of the most powerful things I see in horses is their ability to mirror us as humans. They will physically represent many of our emotions, when they are connected to us. And they often seem to have an uncanny ability to present what we are dealing with. For example, I just recently watched a horse literally push around someone who was talking about feeling pushed around in her life. They present an opportunity to face a challenge that is too scary to face with adults.
Upon completion of graduate school, honestly, I just wanted to take Shadow to work with me. So, I got her certified as a therapy dog, and over the next few years, she went to work with me at two different treatment centers. I quickly realized that her own skittishness and avoidance of contact was a wonderful conduit for helping those who had experienced trauma to see that their reactions were normal. Shadow never was the cuddly dog one might expect of a therapy animal; many of my clients never really got that physically close to her. But, I was repeatedly told of the major impact that she had, and since have been surprised to hear of the number of past clients who chose to get a shiba inu in adulthood.
At times in my career, I have been exposed to equine assisted therapy. And I always saw the potential, and was strongly impacted by the ways it could be beneficial for those with eating disorders. I have begun a training program for a specific type of equine assisted therapy, called Gestalt Equine Psychotherapy, and I have a new partner in crime, Daisy (or if we are feeling particularly elaborate: Miss Daisy Mae). I thought I'd talk some about the connections I see between equine therapy and eating disorder treatment, and I'd love to hear others' thoughts about this. Reality is that equine assisted therapy is not a highly researched field. There's not a lot of concrete data to back it, but those who do it know intuitively it's effectiveness, and those who experience it are often blown away by how powerful it is. So, why equine assisted therapy in eating disorder treatment? These are my initial thoughts:
 1. In my opinion, "the best" equine assisted therapy is about the relationship with the horse. It is not using the horse as a "tool," but instead as a co-therapist. Eating disorders have the impact of disconnection, from oneself and from others. For various reasons, human relationships can become threatening, yet that with an animal can be safe. The horse as co-therapist can help facilitate reconnection: with one's emotions, with one's physical body, with relationships in general, and with others in the client's life. When one has an eating disorder, they often cut themselves off from the head down. The body is often ignored at best, and rejected at worst. Well, imagine trying to engage on the ground with a very large animal, without being present in one's body. To take it one step further, imagine trying to sit upon a horse, or ride a horse, without being connected. As you can imagine, these things would be very difficult, so interaction with a horse can challenge that disconnection in very real, and powerful, ways.
1. In my opinion, "the best" equine assisted therapy is about the relationship with the horse. It is not using the horse as a "tool," but instead as a co-therapist. Eating disorders have the impact of disconnection, from oneself and from others. For various reasons, human relationships can become threatening, yet that with an animal can be safe. The horse as co-therapist can help facilitate reconnection: with one's emotions, with one's physical body, with relationships in general, and with others in the client's life. When one has an eating disorder, they often cut themselves off from the head down. The body is often ignored at best, and rejected at worst. Well, imagine trying to engage on the ground with a very large animal, without being present in one's body. To take it one step further, imagine trying to sit upon a horse, or ride a horse, without being connected. As you can imagine, these things would be very difficult, so interaction with a horse can challenge that disconnection in very real, and powerful, ways.2. Trust: Let's face it; horses are at least 900 pounds, and taller than us. They physically present a challenge to trust. But they will quickly illustrate the desire and motivation to trust us as humans. And that can be so powerful to those who have learned to distrust others.

3. Mirroring: One of the most powerful things I see in horses is their ability to mirror us as humans. They will physically represent many of our emotions, when they are connected to us. And they often seem to have an uncanny ability to present what we are dealing with. For example, I just recently watched a horse literally push around someone who was talking about feeling pushed around in her life. They present an opportunity to face a challenge that is too scary to face with adults.
4. Presence: This is very similar to the connection piece. But those with eating disorders, almost without fail, have high anxiety. They are often lost in their thoughts, overwhelmed by their fears and worries. Being in the presence of a horse challenges that. If you don't engage with a horse, and be present with them, they will literally turn and walk away. But, if the client become present, the horse will engage. This can be a powerful illustration of what happens in human relationships in the life of someone with an eating disorder.
5. Communication: Those with EDs often become silent, not saying what they are thinking and feeling. A horse, or a dog, can present a safe environment for beginning to open up again, and then a safe partner for beginning to talk to people whom the client might find more threatening.
I am really interested to hear what thoughts others might have regarding the overlap between equine assisted psychotherapy and eating disorder treatment! This work is being done in inpatient and residential settings a lot, but perhaps is less common outpatient. I am excited to see this area of eating disorder treatment continue to expand.
Thursday, October 3, 2013
Insurance Coverage for Eating Disorders--a year later
Imagine my surprise when I looked back at the history of posts, and noticed I posted on October 4, 2012, about insurance coverage for eating disorder treatment. I then looked down at my watch and confirmed, it is in fact October 3, 2013 today. Very strange.
What I'm sad to report is that this remains a very real battle for individuals needing eating disorder treatment. There is movement on the national and state level to advocate for better coverage, but the progress is slow. I wanted to share a recent story to highlight this battle, and then provide some ideas of things you can do.
Over the past few months, a family has been battling their teenager's eating disorder at home. This teen had sought inpatient/residential treatment previously, and was discharged as soon as his benefits were exhausted. The parents could not afford the high costs of ongoing residential care on their own, which is true for most families. The only likely outcome came to fruition. The teenager relapsed and I met the family a few weeks later. The teen was admitted to the hospital, which began to fight the insurance company for ongoing benefits. I have never seen a hospital phrase their concerns so strongly, including repeatedly referring to the teen's situation as "life-threatening." The hospital went through many appeals, yet insurance continued to deny coverage for anything other than outpatient care. This was a teenager who was not medically stable to be in outpatient care, and, without a doubt, met criteria for inpatient. But, in the end insurance won, and the teen and family were discharged and returned for outpatient treatment.
This situation highlights a number of concerns about the role of insurance companies in eating disorder treatment. In this case, an insurance reviewer determined the care that this very sick teenager could receive. Of course, we can all make the argument that in the end it was the parents' decision, but is it really a decision, for the average family, when their option is to pay $30,000+/month, out of pocket, for inpatient treatment? Certainly, the insurance company made the argument over and over that it was "not their fault." "The benefit is exhausted," they proclaimed. Yet, every insurance company has the option of providing additional coverage when the need arises, if they choose. Some will choose to do so; clearly, others will not.
So, what can you do when you find yourself trying to battle an insurance company, or insurance policies in general:
What I'm sad to report is that this remains a very real battle for individuals needing eating disorder treatment. There is movement on the national and state level to advocate for better coverage, but the progress is slow. I wanted to share a recent story to highlight this battle, and then provide some ideas of things you can do.
Over the past few months, a family has been battling their teenager's eating disorder at home. This teen had sought inpatient/residential treatment previously, and was discharged as soon as his benefits were exhausted. The parents could not afford the high costs of ongoing residential care on their own, which is true for most families. The only likely outcome came to fruition. The teenager relapsed and I met the family a few weeks later. The teen was admitted to the hospital, which began to fight the insurance company for ongoing benefits. I have never seen a hospital phrase their concerns so strongly, including repeatedly referring to the teen's situation as "life-threatening." The hospital went through many appeals, yet insurance continued to deny coverage for anything other than outpatient care. This was a teenager who was not medically stable to be in outpatient care, and, without a doubt, met criteria for inpatient. But, in the end insurance won, and the teen and family were discharged and returned for outpatient treatment.
This situation highlights a number of concerns about the role of insurance companies in eating disorder treatment. In this case, an insurance reviewer determined the care that this very sick teenager could receive. Of course, we can all make the argument that in the end it was the parents' decision, but is it really a decision, for the average family, when their option is to pay $30,000+/month, out of pocket, for inpatient treatment? Certainly, the insurance company made the argument over and over that it was "not their fault." "The benefit is exhausted," they proclaimed. Yet, every insurance company has the option of providing additional coverage when the need arises, if they choose. Some will choose to do so; clearly, others will not.
So, what can you do when you find yourself trying to battle an insurance company, or insurance policies in general:
- Lisa Kantor, of Kantor and Kantor, is an attorney in California that is well-loved within the eating disorder community. She is taking on insurance companies and fighting for appropriate coverage for eating disorder patients. So, consider contacting her to see if she can help with your case.
- Appeal, appeal, appeal. You shouldn't HAVE TO fight this hard, but reality is that if you battle the insurance company enough, they often will eventually listen. The squeaky wheel, and all that.
- If the eating disorder has resulted in medical complications, make sure hospitals and treatment centers are billing under medical codes, when possible. So, rather than billing for anorexia, they would bill for the medical sequelae: hypothermia, bradycardia, orthostatic hypotension. Even if the treatment has already been billed under an eating disorder, ask them to correct the bill, providing the medical diagnoses instead. This will mean your medical benefits are used, not mental health.
- Research the mental health parity laws in your state and make sure the insurance company is in compliance with these.
- Contact your legislators and make them aware of the need to address appropriate coverage for eating disorders. Ask them to review legislation in other states, or at the national level, and propose similar legislation in your state.
- Ask the insurance company to flex your benefits. An example might be that you have 10 inpatient days, which generally can be flexed to greater partial (PHP/day treatment) days, and even more additional outpatient days.
- Ask your physician to provide a referral for dietitians and therapists, making it clear the physicians sees these services as paramount to the patient's care.
I'm sure there are other ideas that have worked for others. Please, if you have had success battling an insurance company, share what has worked for you.
Honor Your Hunger
by: Nicole Holt, RD, CD
Hunger has helped mankind
survive since the beginning of time. Without
a primal drive to seek food in times of need, the human species would have
ceased to exist. This is why statements like, “I am an awful person because I overate,” or “I ate this food because I don’t have any control,” are misguided and unhelpful.
It may come as a surprise, but the body doesn’t respond to shoulds and food
rules. Our body has a process that is remarkably efficient when we let it do
its job without interfering.
During
the day your body gauges a number of things including blood sugar levels,
hormone levels, and stretch receptors in the stomach. If levels vary from
acceptable, and the stomach is empty, your brain triggers the hunger response. If we refuse to eat intuitively, by
either under eating or ignoring hunger signals, our digestive system interprets
the lack of nutrition as starvation. When our body realizes the energy deficit, it
fights back by causing extreme hunger, anxiety, dizziness, crankiness, etc to
protect against the effects of malnutrition. We may interpret these signals as lack of willpower and drive, when in reality our organs are working hard to combat
starvation.
The
authors of Intuitive Eating have this
to say about honoring your hunger:
“Keep your body fed biologically
with adequate energy and carbohydrates. Otherwise, you can trigger a primal
drive to overeat. Once you reach the moment of excessive hunger, all intentions
of moderate, conscious eating are fleeting and irrelevant. Learning to honor
this first biological signal sets the stage for rebuilding trust with yourself
and food”.
In other words, to avoid chaotic
eating you must do something that feels completely counter intuitive--eat!
Some helpful tools for preventing
hunger include:
- Checking in with yourself every couple of hours to gauge your hunger and then acting upon it if needed
- Combining carbohydrates and protein sources for energy and lasting satiety
- Planning meals and snacks ahead of time
- Keeping snacks on hand in case of hunger
For most people, the most distressing eating disorder behavior is overeating or bingeing. Hopefully this information helps to clarify the role under eating or dieting plays in leading to these behaviors and helps motivate you to honor your hunger!
Wednesday, July 31, 2013
The Job of a Therapist
A therapist's job is an odd one. In fact, my job is officially to work myself out of a job. Weird, huh? But true. My job is to support people in "getting better," however that is defined, and then watch them walk away. When I started this blog, it was called Within Four Walls, because part of what I wanted to be able to communicate was the power, and for me, joy, of working with people with eating disorders. A couple years ago, I was at a local gathering of people who treated or wanted to treat eating disorders, and I was appalled when I heard a therapist state, "Oh, nobody with an eating disorder ever gets better anyway." I had to bite back my desire to tell her to never, ever see another eating disorder patient. But, that is an a common misconception; that eating disorders are generally untreatable. So not true.
Recently, I had a final session with a woman who I have been working with for years. Obviously, I don't want to disclose details about this woman, but also want to say enough for you, the reader, to understand why the statement that people with eating disorders don't get better is so wrong. When I met this woman, she was a shell of a person, in every way.
Today, she left to move to another place to start a graduate program. And, when you hang out with someone every week, or so, for a few years, you lose track of all the changes that happen. It's not until you look back at where things started that it really strikes you, the therapist, just how much changed. I'm sure if anyone were going to, this woman fit the profile of the person who would "never get better." The severity of the illness and it's impact on her physiology, the overall impairment in functioning in her life; there was a lot going against her. When I look back, I see that it didn't look good all those years ago. But, years passed, and in reality, she has been recovered from her eating disorder for years. It has not been the focus on her therapy work for a long time and many situations have shown she truly is in recovery. Therapy became about life and rebuilding, and she did.
In the final session, she tried to give me the primary responsibility for "getting her better." Nope, that wasn't going to happen! It wasn't me. So, what was it? Well, first it was that she wanted to get better. She started the process, she continued the process, she hung in there through hairy moments and good. She drove the process. If you really think about it, what is eating disorder treatment? Sure, to a certain extent we help people "re-learn how to eat." But, really, everyone KNOWS how to eat. We don't have super Jedi mind tricks that somehow make someone eat again.
So, what is it that we do? If you look at psychology, and therapy in general, I'd hate to even try to count the number of approaches that us therapists can be trained in. There's about every cute little combination of letters in the book, all labeling some therapeutic approach that is destined to be the NEXT, BEST THING!
But a couple years ago, when I was panicking about a patient and whether I was doing things "right," and was told by some clinicians that I was doing things wrong, another clinician pointed out the research that basically says that we as therapists can do almost anything, within reason, and as long as we believe it works, and then our patients believe it works; well, it tends to work.
So, you take all those therapy approaches....CBT, IPT, DBT, ACT, ABCDEFG (that's not really one), and they all work, really. But what I believe works, what I believe therapy offers people, is a relationship. That's what therapy is, and that's what we, as people, need (except, as I always tell my clients, there is this guy that lives in a cave outside of Nederland, CO...or at least he did when I was in grad school...and there are a few people like him that seem to not need relationships....but those folks are rare). So, that's what I offered to this woman. I did not "make her better." I gave her a relationship, and she chose to use that relationship to change her life. And, in my experience, the change that comes from the power of the relationship is long-standing. So, I don't worry that she will return to her eating disorder. I truly believe she is recovered. And that puts a huge smile on my face, knowing where things started. She chose her life over her eating disorder.
So, I was reminded by this patient the true power of what happens Within these, and all other, Four Walls.
Recently, I had a final session with a woman who I have been working with for years. Obviously, I don't want to disclose details about this woman, but also want to say enough for you, the reader, to understand why the statement that people with eating disorders don't get better is so wrong. When I met this woman, she was a shell of a person, in every way.
Today, she left to move to another place to start a graduate program. And, when you hang out with someone every week, or so, for a few years, you lose track of all the changes that happen. It's not until you look back at where things started that it really strikes you, the therapist, just how much changed. I'm sure if anyone were going to, this woman fit the profile of the person who would "never get better." The severity of the illness and it's impact on her physiology, the overall impairment in functioning in her life; there was a lot going against her. When I look back, I see that it didn't look good all those years ago. But, years passed, and in reality, she has been recovered from her eating disorder for years. It has not been the focus on her therapy work for a long time and many situations have shown she truly is in recovery. Therapy became about life and rebuilding, and she did.
In the final session, she tried to give me the primary responsibility for "getting her better." Nope, that wasn't going to happen! It wasn't me. So, what was it? Well, first it was that she wanted to get better. She started the process, she continued the process, she hung in there through hairy moments and good. She drove the process. If you really think about it, what is eating disorder treatment? Sure, to a certain extent we help people "re-learn how to eat." But, really, everyone KNOWS how to eat. We don't have super Jedi mind tricks that somehow make someone eat again.
So, what is it that we do? If you look at psychology, and therapy in general, I'd hate to even try to count the number of approaches that us therapists can be trained in. There's about every cute little combination of letters in the book, all labeling some therapeutic approach that is destined to be the NEXT, BEST THING!
But a couple years ago, when I was panicking about a patient and whether I was doing things "right," and was told by some clinicians that I was doing things wrong, another clinician pointed out the research that basically says that we as therapists can do almost anything, within reason, and as long as we believe it works, and then our patients believe it works; well, it tends to work.
So, you take all those therapy approaches....CBT, IPT, DBT, ACT, ABCDEFG (that's not really one), and they all work, really. But what I believe works, what I believe therapy offers people, is a relationship. That's what therapy is, and that's what we, as people, need (except, as I always tell my clients, there is this guy that lives in a cave outside of Nederland, CO...or at least he did when I was in grad school...and there are a few people like him that seem to not need relationships....but those folks are rare). So, that's what I offered to this woman. I did not "make her better." I gave her a relationship, and she chose to use that relationship to change her life. And, in my experience, the change that comes from the power of the relationship is long-standing. So, I don't worry that she will return to her eating disorder. I truly believe she is recovered. And that puts a huge smile on my face, knowing where things started. She chose her life over her eating disorder.
So, I was reminded by this patient the true power of what happens Within these, and all other, Four Walls.
Wednesday, July 17, 2013
What should my child weigh?
As I was thinking more about the last post, I realized I wanted to share some more information related to kids and their weights. I'll begin with a story:
A few weeks ago, I was talking to a physician about a referral. He let me know that this teenager had lost a significant amount of weight....I'll make up numbers here....let's say she was 5'2 and 120# prior to her weight loss. She lost to 100#, was admitted to the hospital, partially refed, and now will be seen for outpatient follow up. The doctor's stance as not uncommon, and amounted to this: We'll say she gained to 110# in the hospital and this is her new "goal weight," because, in his words, 110# is a reasonable weight for a teenager that is 5'2.
And for me, there's the internal sigh, knowing there's little I can do to override this physician's understanding of appropriate weight, or eating disorder terms, "goal weight." Reality is that very few health professionals, of any discipline, have the opportunity to learn about eating disorder treatment while in training. The main way of learning about ED treatment is through specialty rotations or job placements. So, sadly, the norm is that health professionals are more strongly influenced by the media, and thus the diet industry, than by solid science.
So, everyone knows about those lovely height/weight tables, right? Pick an age, pick a height, and voila! A piece of paper will tell you what you should ideally weight. Okay, well, the name for that table is the MetLife Height/Weight table, and yep, MetLife is an insurance company. So, these were tables designed by an insurance company to protect their interests, and are based in the (flawed) theory that lower weight has lower health consequences. Which is actually completely incorrect, but that's a whole 'nother post.
The theory here is that we can take ALL THE HUMANS IN THE WORLD, and a piece of paper should tell us what we SHOULD weigh. (I hope the sarcasm here is palpable!). This is illogical. So, if you follow that handy dandy piece of paper, yes, the doctor's statement above is "correct." Because that table will say about 5'2, 110# for a female. The problem here is that this particular teenager was at 120# prior to her disorder, so what is to say she SHOULD now weigh less as a result of having a disorder.
What's the real answer?
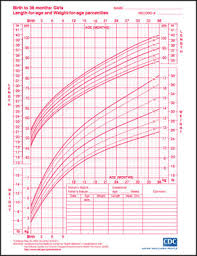 It's really pretty straightforward, though it does involve another handy dandy piece of paper. The new piece of paper is a CDC Growth Chart for boys or girls. Each time your child sees his/her pediatrician, height and weight is recorded on one of these charts. In my experience, most kids will actually track pretty well along a particular percentile in height and in weight.
It's really pretty straightforward, though it does involve another handy dandy piece of paper. The new piece of paper is a CDC Growth Chart for boys or girls. Each time your child sees his/her pediatrician, height and weight is recorded on one of these charts. In my experience, most kids will actually track pretty well along a particular percentile in height and in weight.
So, let's make our female teenager above 14 years old. At 120#, she would be in the 25%ile for height and I'll say 62%ile for weight (this is a rough estimate just eyeballing the chart). So, let's say she lost weight and then was hospitalized and now at age 15, she is entering outpatient treatment at 110#. Reality is that her height likely remained the same, because maintaining too low a weight stunts height, which, again, is a whole 'nother post. But, at 15, 110# puts her at the 33rd-ish percentile.
Assuming this teenager had tracked at the 55th-65th percentile throughout her childhood, to now say she is healthy in the 33rd percentile, simply because a height/weight chart says that is good, is irrational. Teenagers are supposed to continue to gain, both in height and weight. But, unfortunately, health professionals, and then parents, often think the child/teenager is "fine" as long as he/she meets the cultural expectations for weight.
To get my point across solidly, let's say that there's a handy dandy MetLife chart for shoe size, or even height for age. So, let's say that at age 16, the chart says I should be 5'4 (average height for women), and a shoe size of 7.5. Well, good news! My shoe size actually is 7.5, so woo hoo! I did it! But, sadly, I suffer from height failure, and am only 5'2 (or 5'3, if the doctor is being kind). But the chart says I need to be 5'4....so, I guess I better get stretching. I better have someone pull on my hands and someone else pull on my legs until I get there, right? Ouch.
That sounds nutty when it comes to height. But my point is that it is equally nutty when it comes to weight. If a child/teen has always tracked at the 95%ile for height or weight, then they are HEALTHY at 95%ile, even if our society begs to differ. And, if they have always tracked at the 5th%ile, then they are HEALTHY there, which our society fully supports, at least with respect to weight.
Now, parents, please do not now go demand your child's height/weight records from their pediatrician. You don't need to drive yourself nuts analyzing it. Just know that that reference point is available, and is much more accurate than a chart created by an insurance company. Parents, keep your focus on helping your child eat when he/she is hungry and stop when he/she is full. If your child does this, he/she will maintain his/her natural weight, well, naturally.
But, health professionals, if you are relying on the MetLife tables, or the other handy dandy estimates that are out there, please reconsider. Humans should be judged against their own history (growth charts), not an average of people put into table form (MetLife Height/Weight chart).
A few weeks ago, I was talking to a physician about a referral. He let me know that this teenager had lost a significant amount of weight....I'll make up numbers here....let's say she was 5'2 and 120# prior to her weight loss. She lost to 100#, was admitted to the hospital, partially refed, and now will be seen for outpatient follow up. The doctor's stance as not uncommon, and amounted to this: We'll say she gained to 110# in the hospital and this is her new "goal weight," because, in his words, 110# is a reasonable weight for a teenager that is 5'2.
And for me, there's the internal sigh, knowing there's little I can do to override this physician's understanding of appropriate weight, or eating disorder terms, "goal weight." Reality is that very few health professionals, of any discipline, have the opportunity to learn about eating disorder treatment while in training. The main way of learning about ED treatment is through specialty rotations or job placements. So, sadly, the norm is that health professionals are more strongly influenced by the media, and thus the diet industry, than by solid science.
So, everyone knows about those lovely height/weight tables, right? Pick an age, pick a height, and voila! A piece of paper will tell you what you should ideally weight. Okay, well, the name for that table is the MetLife Height/Weight table, and yep, MetLife is an insurance company. So, these were tables designed by an insurance company to protect their interests, and are based in the (flawed) theory that lower weight has lower health consequences. Which is actually completely incorrect, but that's a whole 'nother post.
The theory here is that we can take ALL THE HUMANS IN THE WORLD, and a piece of paper should tell us what we SHOULD weigh. (I hope the sarcasm here is palpable!). This is illogical. So, if you follow that handy dandy piece of paper, yes, the doctor's statement above is "correct." Because that table will say about 5'2, 110# for a female. The problem here is that this particular teenager was at 120# prior to her disorder, so what is to say she SHOULD now weigh less as a result of having a disorder.
What's the real answer?
So, let's make our female teenager above 14 years old. At 120#, she would be in the 25%ile for height and I'll say 62%ile for weight (this is a rough estimate just eyeballing the chart). So, let's say she lost weight and then was hospitalized and now at age 15, she is entering outpatient treatment at 110#. Reality is that her height likely remained the same, because maintaining too low a weight stunts height, which, again, is a whole 'nother post. But, at 15, 110# puts her at the 33rd-ish percentile.
Assuming this teenager had tracked at the 55th-65th percentile throughout her childhood, to now say she is healthy in the 33rd percentile, simply because a height/weight chart says that is good, is irrational. Teenagers are supposed to continue to gain, both in height and weight. But, unfortunately, health professionals, and then parents, often think the child/teenager is "fine" as long as he/she meets the cultural expectations for weight.
To get my point across solidly, let's say that there's a handy dandy MetLife chart for shoe size, or even height for age. So, let's say that at age 16, the chart says I should be 5'4 (average height for women), and a shoe size of 7.5. Well, good news! My shoe size actually is 7.5, so woo hoo! I did it! But, sadly, I suffer from height failure, and am only 5'2 (or 5'3, if the doctor is being kind). But the chart says I need to be 5'4....so, I guess I better get stretching. I better have someone pull on my hands and someone else pull on my legs until I get there, right? Ouch.
That sounds nutty when it comes to height. But my point is that it is equally nutty when it comes to weight. If a child/teen has always tracked at the 95%ile for height or weight, then they are HEALTHY at 95%ile, even if our society begs to differ. And, if they have always tracked at the 5th%ile, then they are HEALTHY there, which our society fully supports, at least with respect to weight.
Now, parents, please do not now go demand your child's height/weight records from their pediatrician. You don't need to drive yourself nuts analyzing it. Just know that that reference point is available, and is much more accurate than a chart created by an insurance company. Parents, keep your focus on helping your child eat when he/she is hungry and stop when he/she is full. If your child does this, he/she will maintain his/her natural weight, well, naturally.
But, health professionals, if you are relying on the MetLife tables, or the other handy dandy estimates that are out there, please reconsider. Humans should be judged against their own history (growth charts), not an average of people put into table form (MetLife Height/Weight chart).
"The Childhood Obesity Epidemic" and Eating Intuitively
Our society has done a wonderful job scaring everyone about rates of childhood obesity. I haven't delved into the research myself and really looked at the extent to which children are at higher weights/BMIs, etc., but I feel confident that the way our society is responding to any issues that might be present is not that beneficial. Parents are learning they need to restrict their child's food intake and access to food. They are advised by doctors, therapists, and the media, to limit what their child has access to and control food intake.
But let's think about this. Go back to being a child or teenager. Think of what happened when your parents told you you couldn't do something, and particularly when they told you you couldn't do something that all your friends were doing. Right, you rebelled against that, or at least thought about it.
So, when, as a parent, you try to limit your child's access to soda, fast food, pizza, "junk food," etc., the greater risk is that you will accomplish pushing your child towards those foods as they fight back against the restriction. The diet industry, and thus most health professionals, will identify all these foods as "bad." We are instructed to not eat them, and it is implied that it is "bad" if we do. The shame is compounded when it is then implied that to allow access to these foods is "bad" and that having a child eat these foods, especially when they more than society says is idea is "bad." That's a lot of "bad"s, for both parent and child.
It is true that not all foods offer the same nutritional value. Yes, there are limits, and sometimes significant limits, to the nutritional value of the foods that have been identified as bad. However, these foods are present in our world, and the black and white view of "don't eat them" isn't very likely to work out well. So what is a parent to do instead?
Rather than focusing heavily on the foods that your child is eating, focus instead on their hunger and fullness level. Kids are born intuitive eaters. Your babies and young children ate intuitively. They asked for food when they were hungry, and they stopped eating when they were full. They didn't have the neuroses we adults have about foods because, to kids, food is just food. However, as they grow up in our culture and hear about good and bad foods, and external forces begin to impact when they start and stop eating, they lose their ability to follow their hunger and fullness cues. Telling your child she has to eat everything on her plate overrides her fullness cues. Telling your child he cannot eat, or cannot eat ____ when he's hungry overrides his hunger cues. But you can help your kids go back to those cues by talking to them not about the food, but instead about how hungry and full they are.
How does this look? You are concerned your child is overeating, so you ask him whether he's still hungry. If he says yes, you cannot know for sure whether that is the truth, but you can know that you are helping him to think about that factor. Over time, he is more likely to think about this variable when he is making food choices. It will help if this is how you approach food yourself so it is modeled for your child.
It's not as much about what he/she is eating, but the physical cues that are driving the eating behavior. If you focus on what and how much he/she eats, your child is more likely to feel criticized and blamed, particularly if he/she actually is eating due to hunger! Certainly, have foods with high nutritional value available to your kids, and serve these foods. But, I think we all know that there are times when fast food is what is most available, and really, in the end, fast food is a source of protein, carbs, fat, and more so recently, fruits and vegetables. So, it doesn't have to be a big deal. It's not ideal to eat them all the time, but reality is that it also is not a good idea to eat broccoli all the time (I don't know why; I always pick on broccoli! I just have a vendetta against that little green tree....) Eating any one source of food repeatedly limits nutrition, so eat fast food, and broccoli, as part of a varied diet, and you will be fine.
I hope, moving forward, parents will question more trying to limit their child's food intake. I have seen this result in a variety of eating problems, and what is sad is that it is all well-intended and parents are directed to take these steps by health professionals. Again, remember that your babies and young children were intuitive eaters. Help them return to that if our society has overridden this natural way of being.
But let's think about this. Go back to being a child or teenager. Think of what happened when your parents told you you couldn't do something, and particularly when they told you you couldn't do something that all your friends were doing. Right, you rebelled against that, or at least thought about it.
So, when, as a parent, you try to limit your child's access to soda, fast food, pizza, "junk food," etc., the greater risk is that you will accomplish pushing your child towards those foods as they fight back against the restriction. The diet industry, and thus most health professionals, will identify all these foods as "bad." We are instructed to not eat them, and it is implied that it is "bad" if we do. The shame is compounded when it is then implied that to allow access to these foods is "bad" and that having a child eat these foods, especially when they more than society says is idea is "bad." That's a lot of "bad"s, for both parent and child.
It is true that not all foods offer the same nutritional value. Yes, there are limits, and sometimes significant limits, to the nutritional value of the foods that have been identified as bad. However, these foods are present in our world, and the black and white view of "don't eat them" isn't very likely to work out well. So what is a parent to do instead?
Rather than focusing heavily on the foods that your child is eating, focus instead on their hunger and fullness level. Kids are born intuitive eaters. Your babies and young children ate intuitively. They asked for food when they were hungry, and they stopped eating when they were full. They didn't have the neuroses we adults have about foods because, to kids, food is just food. However, as they grow up in our culture and hear about good and bad foods, and external forces begin to impact when they start and stop eating, they lose their ability to follow their hunger and fullness cues. Telling your child she has to eat everything on her plate overrides her fullness cues. Telling your child he cannot eat, or cannot eat ____ when he's hungry overrides his hunger cues. But you can help your kids go back to those cues by talking to them not about the food, but instead about how hungry and full they are.
How does this look? You are concerned your child is overeating, so you ask him whether he's still hungry. If he says yes, you cannot know for sure whether that is the truth, but you can know that you are helping him to think about that factor. Over time, he is more likely to think about this variable when he is making food choices. It will help if this is how you approach food yourself so it is modeled for your child.
It's not as much about what he/she is eating, but the physical cues that are driving the eating behavior. If you focus on what and how much he/she eats, your child is more likely to feel criticized and blamed, particularly if he/she actually is eating due to hunger! Certainly, have foods with high nutritional value available to your kids, and serve these foods. But, I think we all know that there are times when fast food is what is most available, and really, in the end, fast food is a source of protein, carbs, fat, and more so recently, fruits and vegetables. So, it doesn't have to be a big deal. It's not ideal to eat them all the time, but reality is that it also is not a good idea to eat broccoli all the time (I don't know why; I always pick on broccoli! I just have a vendetta against that little green tree....) Eating any one source of food repeatedly limits nutrition, so eat fast food, and broccoli, as part of a varied diet, and you will be fine.
I hope, moving forward, parents will question more trying to limit their child's food intake. I have seen this result in a variety of eating problems, and what is sad is that it is all well-intended and parents are directed to take these steps by health professionals. Again, remember that your babies and young children were intuitive eaters. Help them return to that if our society has overridden this natural way of being.
Monday, June 24, 2013
Making sense of your disorder
The really good news is that those in treatment for an eating disorder eventually reach that day where they walk in and say that they feel as though their eating disorder is only a small part of his/her life. These are the wonderful days as an eating disorder therapist!
But, what is one to do when that day has been reached. Some look at me and think they no longer are allowed to come see me because I "treat eating disorders." But, no, treating eating disorders is, in the end, just like treating any other issue. It is really about what was underlying the eating disorder all along.
So, do you just stop talking about the eating disorder altogether? Now what?! I think there are a couple questions that can be really helpful to address:
1. At the beginning, it is the most useless question, as almost nobody can answer it; however, by the end, I like to have patients explain to me what their eating disorder was about. This allows them to develop a cohesive understanding of how the ED "helped them" and sets the stage for #2.
2. Given this understanding, what situations in the future are most likely to set you up to relapse?, and
3. What are the "red flags," or early warning signs, that the ED is returning?
Answering these questions can help create a sense of control and power if and when the ED starts to creep back into one's life, and as I tell all my patients, once the ED is understood, it loses a lot of power. It's hard to know EXACTLY what is going on and still do it again; not impossible, but harder. It makes the behavior less effective, which decreases the chances of returning to it. Everyone will face stressors again in life, and the ED will always be a choice. But in my experience, many patients will have developed new coping skills, and whereas they will think ED thoughts again, they do not engage in the behaviors. Or if they do, they catch it early, and choose differently.
There's a lot more hope about recovery from an eating disorder than many seem to think. And it is amazing to see it happen.
But, what is one to do when that day has been reached. Some look at me and think they no longer are allowed to come see me because I "treat eating disorders." But, no, treating eating disorders is, in the end, just like treating any other issue. It is really about what was underlying the eating disorder all along.
So, do you just stop talking about the eating disorder altogether? Now what?! I think there are a couple questions that can be really helpful to address:
1. At the beginning, it is the most useless question, as almost nobody can answer it; however, by the end, I like to have patients explain to me what their eating disorder was about. This allows them to develop a cohesive understanding of how the ED "helped them" and sets the stage for #2.
2. Given this understanding, what situations in the future are most likely to set you up to relapse?, and
3. What are the "red flags," or early warning signs, that the ED is returning?
Answering these questions can help create a sense of control and power if and when the ED starts to creep back into one's life, and as I tell all my patients, once the ED is understood, it loses a lot of power. It's hard to know EXACTLY what is going on and still do it again; not impossible, but harder. It makes the behavior less effective, which decreases the chances of returning to it. Everyone will face stressors again in life, and the ED will always be a choice. But in my experience, many patients will have developed new coping skills, and whereas they will think ED thoughts again, they do not engage in the behaviors. Or if they do, they catch it early, and choose differently.
There's a lot more hope about recovery from an eating disorder than many seem to think. And it is amazing to see it happen.
Thursday, May 30, 2013
Anger a key part of recovery?
Sometimes, things become readily apparent when maybe they were not as clear before. All along, I have known it is likely very important for those with eating disorders to become angry at their disorder. I don't think I realized until tonight, however, how vital it might be to recovery.
Thursday night is group night. And through many twists and turns, tonight focused on anger. Anger at many things, and perhaps even more important, the struggles these women have with expressing anger. Oh, they feel it; that I don't doubt. But, they struggle to express it, feel comfortable with it, have it be okay. What stood out to me is while trying to get one member to realize that perhaps anger is important in her recovery, another group member provided an example of how the "healthy voice" and "ED voice" might communicate based on whether or not the healthy voice was angry at the ED. So, in the first situation, there was no anger, and the healthy voice was asked to identify what it would say to the ED.
She threw her arms open wide and said something along the lines of, "Come on in!" in a cheerful, welcoming voice.
Then, she was instructed that she, the healthy voice, was mad at the ED. And, I will confess, I don't remember exactly what she said, but I do remember the motion of her hand represented a WWE beat down. I think she might have said something like, "Get out of my house!"
I don't know if the message sunk in, but it sure did to me. It made it even more clear to me how important anger at the ED is if one wants to get better. After all, if you aren't angry at what it has taken from you, what is there to fight?
So, whether it's an ED, or any other negative force in your life, are you opening your arms wide and welcoming it in? Or are you preparing for a (figurative) beat down?
What makes you angry with your eating disorder?
Thursday night is group night. And through many twists and turns, tonight focused on anger. Anger at many things, and perhaps even more important, the struggles these women have with expressing anger. Oh, they feel it; that I don't doubt. But, they struggle to express it, feel comfortable with it, have it be okay. What stood out to me is while trying to get one member to realize that perhaps anger is important in her recovery, another group member provided an example of how the "healthy voice" and "ED voice" might communicate based on whether or not the healthy voice was angry at the ED. So, in the first situation, there was no anger, and the healthy voice was asked to identify what it would say to the ED.
She threw her arms open wide and said something along the lines of, "Come on in!" in a cheerful, welcoming voice.
Then, she was instructed that she, the healthy voice, was mad at the ED. And, I will confess, I don't remember exactly what she said, but I do remember the motion of her hand represented a WWE beat down. I think she might have said something like, "Get out of my house!"
I don't know if the message sunk in, but it sure did to me. It made it even more clear to me how important anger at the ED is if one wants to get better. After all, if you aren't angry at what it has taken from you, what is there to fight?
So, whether it's an ED, or any other negative force in your life, are you opening your arms wide and welcoming it in? Or are you preparing for a (figurative) beat down?
What makes you angry with your eating disorder?
Wednesday, May 29, 2013
From the mouths of interns....
It has been a long time since the last post, and I apologize for that. Things have been very busy, with Utah Center for Eating Disorders formally opening, and the hiring of Nicole Holt, RD. It has been exciting and good change, but comes with growing pains, of course. I have thought often of writing blog posts, but have not made the time. This week, however, I was so overwhelmed by the words of this past year's interns, that I decided trying to summarize their statements was the needed motivation to write again.
One of my passions is doing training and supervision. There is little training in grad school for therapists, dietitians or physicians with regards to ED treatment. I was trained in ED treatment many years ago by a man who was once the top of the field, and then fell, and have always felt that training graduate students or post-docs is my way to give back. I learned many things from this man, and have always referred to him as a brilliant mind who struggled deeply with ethics. Although I cannot say I do much like him, I can say he taught me the concept on which I have built my career and treatment of eating disorders. It was from him that I learned about the physiology underlying eating disorders, and this is what I have strived to teach therapists who want to treat eating disorders. I have been thrilled to have two psychology graduate students "interning" (for those in psychology PhD land, yes, this is the wrong term, but I find it more respectful than "practicum student.") at Utah Center for Eating Disorders.
This week, they passed on their wisdom to this next year's interns. And as I listened to them talk, I realized how many things about ED treatment that slide right past me after years of doing it day in and day out. I will not pretend to quote them, but instead summarize parts of what I heard them say.
They spoke of the awareness of the gravity of the work they were doing. They stated it was some of the most frightening and intimidating work they have done, largely because they learned the physiological impact of the disorders, and accepted the reality that these are the most lethal psychiatric disorders. They spoke of awareness that something could go wrong physically when neither they nor the patient expected it. They spoke of the impact of truly seeing the physical impact, and experiencing deep emotional reactions of sadness and fear as they worked to help those with EDs. I had said to them a couple of times that their reactions really impacted me; through them, I realized "my eyes don't work anymore." I don't see body size as much anymore and react less, simply due to desensitization. It was eye-opening to see EDs again from the perspective of someone who has not been doing the work for so long.
They spoke of the difficulty of taking on more directiveness in patients' lives. After all, in therapy, we are to "accept the client where he/she is at." Well, we cannot do that. We cannot accept an eating disorder, or at least that is my approach. So, we do become more involved, provide more direction, and set some hard lines. It was rewarding to me when they were able to see that this can work, that their patients did not run off and get upset with them for being firm, but instead respected their willingness to jump in and fight against the disorder.
They said many more things, but this cannot be eternal, so I will leave it at that. The bottom line is that working with them and seeing their success in helping patients overcome their disorders was very powerful and rewarding. I learned they were often intimidated by the gravity of the work they were doing; I also learned they were REALLY good at hiding that most of the time!
This is intimidating work, but also incredibly powerful and rewarding. One of the things that irritates me the most is when therapists or other professionals label eating disorders as untreatable. This is far from the truth. And what these two showed was that with a little training, supervision and support, they were able to help their patients change dramatically. And I continue to believe that a major part of that was truly understanding the physiology underlying the disorder. So, if you are a therapist that wants to treat eating disorders, my advice is to prioritize learning the physiology. It goes outside the bounds of typical therapy, but is invaluable. And, as I had to remind them a couple times, past the physiology everything else is "just therapy," and I didn't need to teach them about how to do therapy.
Congratulations Angie and Julia on your internship placements. You will be greatly missed. And welcome on board Kendrick and Larissa! It should be a fun ride!
One of my passions is doing training and supervision. There is little training in grad school for therapists, dietitians or physicians with regards to ED treatment. I was trained in ED treatment many years ago by a man who was once the top of the field, and then fell, and have always felt that training graduate students or post-docs is my way to give back. I learned many things from this man, and have always referred to him as a brilliant mind who struggled deeply with ethics. Although I cannot say I do much like him, I can say he taught me the concept on which I have built my career and treatment of eating disorders. It was from him that I learned about the physiology underlying eating disorders, and this is what I have strived to teach therapists who want to treat eating disorders. I have been thrilled to have two psychology graduate students "interning" (for those in psychology PhD land, yes, this is the wrong term, but I find it more respectful than "practicum student.") at Utah Center for Eating Disorders.
This week, they passed on their wisdom to this next year's interns. And as I listened to them talk, I realized how many things about ED treatment that slide right past me after years of doing it day in and day out. I will not pretend to quote them, but instead summarize parts of what I heard them say.
They spoke of the awareness of the gravity of the work they were doing. They stated it was some of the most frightening and intimidating work they have done, largely because they learned the physiological impact of the disorders, and accepted the reality that these are the most lethal psychiatric disorders. They spoke of awareness that something could go wrong physically when neither they nor the patient expected it. They spoke of the impact of truly seeing the physical impact, and experiencing deep emotional reactions of sadness and fear as they worked to help those with EDs. I had said to them a couple of times that their reactions really impacted me; through them, I realized "my eyes don't work anymore." I don't see body size as much anymore and react less, simply due to desensitization. It was eye-opening to see EDs again from the perspective of someone who has not been doing the work for so long.
They spoke of the difficulty of taking on more directiveness in patients' lives. After all, in therapy, we are to "accept the client where he/she is at." Well, we cannot do that. We cannot accept an eating disorder, or at least that is my approach. So, we do become more involved, provide more direction, and set some hard lines. It was rewarding to me when they were able to see that this can work, that their patients did not run off and get upset with them for being firm, but instead respected their willingness to jump in and fight against the disorder.
They said many more things, but this cannot be eternal, so I will leave it at that. The bottom line is that working with them and seeing their success in helping patients overcome their disorders was very powerful and rewarding. I learned they were often intimidated by the gravity of the work they were doing; I also learned they were REALLY good at hiding that most of the time!
This is intimidating work, but also incredibly powerful and rewarding. One of the things that irritates me the most is when therapists or other professionals label eating disorders as untreatable. This is far from the truth. And what these two showed was that with a little training, supervision and support, they were able to help their patients change dramatically. And I continue to believe that a major part of that was truly understanding the physiology underlying the disorder. So, if you are a therapist that wants to treat eating disorders, my advice is to prioritize learning the physiology. It goes outside the bounds of typical therapy, but is invaluable. And, as I had to remind them a couple times, past the physiology everything else is "just therapy," and I didn't need to teach them about how to do therapy.
Congratulations Angie and Julia on your internship placements. You will be greatly missed. And welcome on board Kendrick and Larissa! It should be a fun ride!
Sunday, February 10, 2013
Announcing: Utah Center for Eating Disorders
I suppose it has been woefully obvious that I have not been posting for a few months. Many things are going on, the largest of which is this announcement! My private practice has now expanded, and will now be known as:
I truly do plan to return to blogging once the dust has settled. Thanks for your patience and support!
I truly do plan to return to blogging once the dust has settled. Thanks for your patience and support!
Eating Disorder Awareness Week 2013
Please join us for the following events:
February 26, 6-7:15pm
Sick of Dieting? A Different Approach to Eating and Weight: Health at Every Size and Intuitive Eating.
Elena Yorgason, RD and Julia Mackaronis, MS
February 27, 6-7pm
You Mean Everyone with and Eating Disorder Isn't Tiny?: Hidden Eating Disorders
Addressing Binge Eating Disorder, Exercise Addiction, Orthorexia
Angela Hicks, PhD
February 28, 6-7:30pm
What can Family and Friends Do? Recovery Panel Discussion
Wendy Hoyt, PhD and Recovery Panel
All presentations will be held at Westminster College, 1840 S. 1300 E, SLC 84105
Health and Wellness Center Special Events Room
We really hope to see everyone there! Please share this information!
February 26, 6-7:15pm
Sick of Dieting? A Different Approach to Eating and Weight: Health at Every Size and Intuitive Eating.
Elena Yorgason, RD and Julia Mackaronis, MS
February 27, 6-7pm
You Mean Everyone with and Eating Disorder Isn't Tiny?: Hidden Eating Disorders
Addressing Binge Eating Disorder, Exercise Addiction, Orthorexia
Angela Hicks, PhD
February 28, 6-7:30pm
What can Family and Friends Do? Recovery Panel Discussion
Wendy Hoyt, PhD and Recovery Panel
All presentations will be held at Westminster College, 1840 S. 1300 E, SLC 84105
Health and Wellness Center Special Events Room
We really hope to see everyone there! Please share this information!
Subscribe to:
Posts (Atom)




